When considering the most important nutrients for pregnant moms, many people immediately think of folic acid, iron, and perhaps Vitamin D. Similarly, when it comes to nutrients crucial for babies starting solids, iron often tops the list. While these are indeed essential, there’s another vital nutrient that deserves attention for its role in growth and development: Omega-3s, particularly DHA.
DHA is essential for brain and eye development in babies, and it supports heart health, mood stability, and cognitive function in moms. Let’s dive into why DHA is so important for both mom and baby.
OMEGA-3S

Not all omega-3 fatty acids are created equal. Among the 11 types, the three most important are ALA, EPA, and DHA.
- Alpha-Linolenic Acid (ALA): ALA is the most common omega-3 fatty acid in the our diet and is primarily found in plant-based sources such as walnuts, seeds (flax, chia, hemp) and oils (canola, soybean, walnut, flaxseed). ALA is a an essential fat because it cannot be made by the body and is needed for normal human growth and development. While ALA can be converted into EPA and DHA, this conversion process is quite inefficient in humans.
- Eicosapentaenoic Acid (EPA): EPA is found primarily in fatty fish and seafood. It plays a significant role in reducing inflammation throughout the body, which is crucial for preventing chronic diseases such as heart disease and arthritis. EPA also has benefits mental health, potentially reducing symptoms of depression.
- Docosahexaenoic Acid (DHA): DHA is a key structural component of the brain, retina, and many other parts of the body. It is essential for brain development and function, making it particularly important during pregnancy and early childhood. DHA can be obtained either through conversion of ALA or directly from food sources rich in DHA, such as fatty fish, seafood or DHA-fortified foods.
THE CONVERSION OF ALA TO DHA
While ALA can be converted into EPA and then DHA, this conversion process, which primarily occurs in the liver, is highly inefficient, with rates reported to be less than 15%.
Additionally, studies have shown that increasing ALA intake during pregnancy does not significantly raise DHA levels in the blood (here, here). Therefore, consuming foods rich in DHA directly (or DHA supplements) is crucial for ensuring an adequate supply of this essential nutrient during pregnancy, supporting both maternal and fetal health effectively.
The active form of DHA found in foods is more beneficial than the converted form from ALA.
WHY IS DHA IMPORTANT DURING PREGNANCY?

DHA plays a crucial role in the development of a fetus’s cell membranes, particularly in the brain and retina. Ensuring adequate DHA intake during pregnancy and the first few years following birth is therefore very important. Prior to birth, the DHA required for proper fetal development is provided by placental transfer from the mother. Following birth, babies must receive DHA through breast milk, formulas fortified with DHA, or DHA supplementation (e.g., fish oil).
- Brain Development: Throughout pregnancy, DHA requirements increase, especially during the third trimester. As pregnancy progresses, maternal blood volume expands, and both the placenta and the developing baby require more DHA. Therefore, DHA is required to support fetal growth and brain development, especially during the third trimester when the fetus undergoes a rapid “brain growth spurt.”
- Eye Development: DHA is also essential for the development of the eyes, as it is the major fatty acid found in the retina, constituting approximately 93% of all omega-3 fatty acids. This high presence of DHA underscores its significance in eye health and visual development.
Studies indicate that during the last trimester, a fetus receives approximately 67 mg of DHA daily from the mother. This requirement increases to 70-80 mg daily during breastfeeding. The substantial demand for DHA during pregnancy and breastfeeding can deplete the mother’s DHA stores to below pre-pregnancy levels by up to 50%, and it can take months to partially replenish these levels. This depletion may pose health risks for the mother, including postpartum depression.
Research has demonstrated that sufficient DHA intake during pregnancy results in several positive outcomes for babies, such as better social behaviour, higher social development scores, enhanced verbal intelligence and reduced risk of pre-term labor, pre-eclampsia, and low birth weight.
RECOMMENDATIONS FOR PREGNANT MOMS
When it comes to recommendations for omega-3s, the guidelines can vary depending on the source. To help clarify, I’ve summarized some of the key recommendations below:
The Ministry of Health Malaysia (RNI)
- 200mg DHA daily
American Pregnancy Association
- 300 mg DHA daily
- Consume 2-3 servings of low mercury fish per week, 8-12 ounces of fatty fish in total.
RECOMMENDATIONS FOR MOMS:
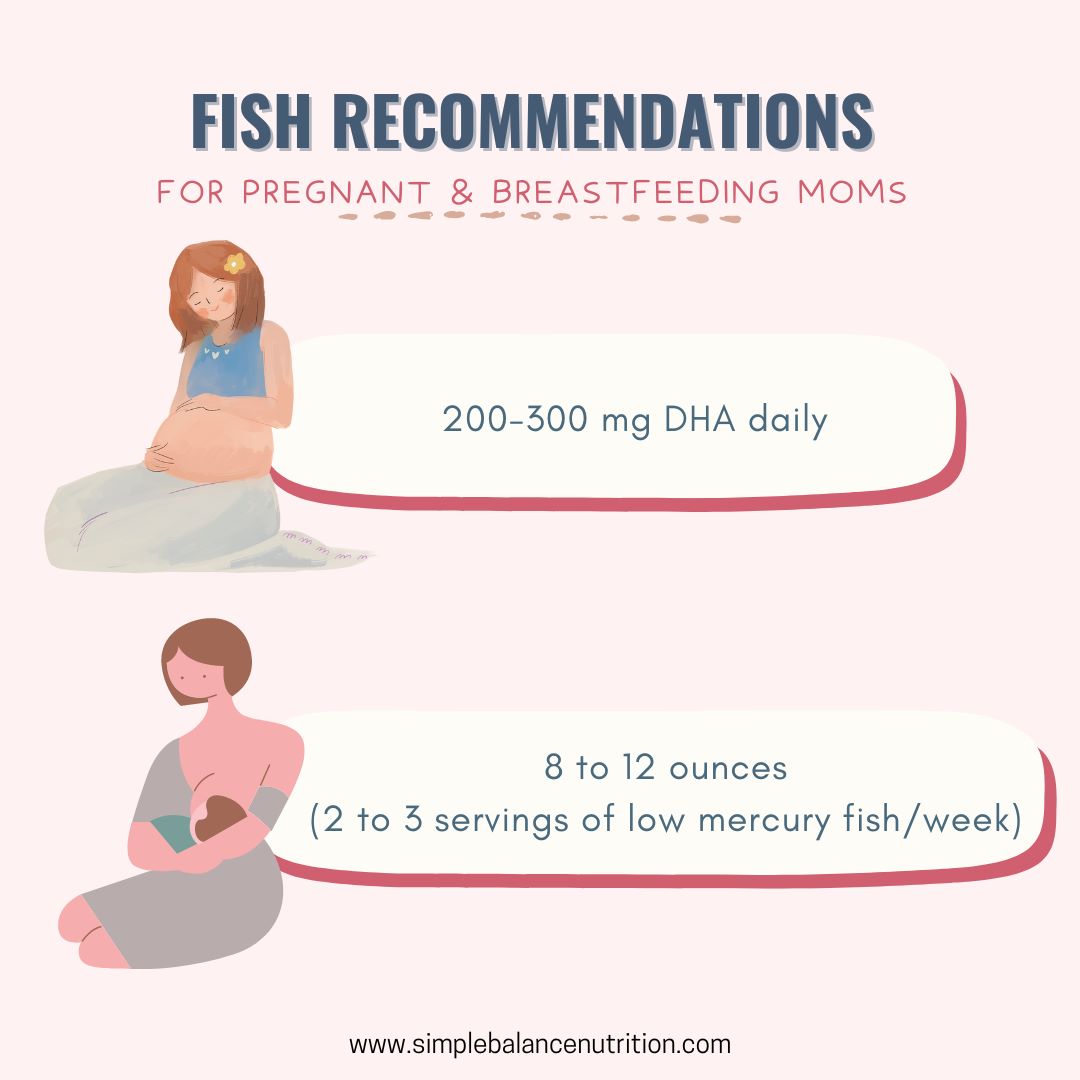
Those who are pregnant or breastfeeding should aim to consume 200 to 300 mg of DHA each day, which means eating 8 to 12 ounces (2 to 3 servings) per week of a variety of fish lower in mercury.
RECOMMENDATIONS FOR BABIES AND TODDLERS
The Institute of Medicine (IOM) has not established specific intake recommendations for EPA and DHA. The current recommendations for total omega-3s intake for babies aged 0-12 months is 0.5g per day, and for toddlers aged 1-3 years old, the recommendation increases to 0.7g ALA per day. These targets can be met if the mother is adhering to her recommended DHA intake and breastfeeding.
American Pregnancy Association
- Infants (1-18 months & < 15 lbs): 32 mg/lb EPA + DHA
- Children (1.5-15 years): 15 mg/lb EPA + DHA
Children should consume two servings of fatty fish per week.
- A serving size is about:
- Ages 1-3 years: 1 ounce
- Ages 4-7 years: 2 ounces
- Ages 8-10 years: 3 ounces
- 11 years and older: 4 ounces
RECOMMENDATIONS FOR CHILDREN:
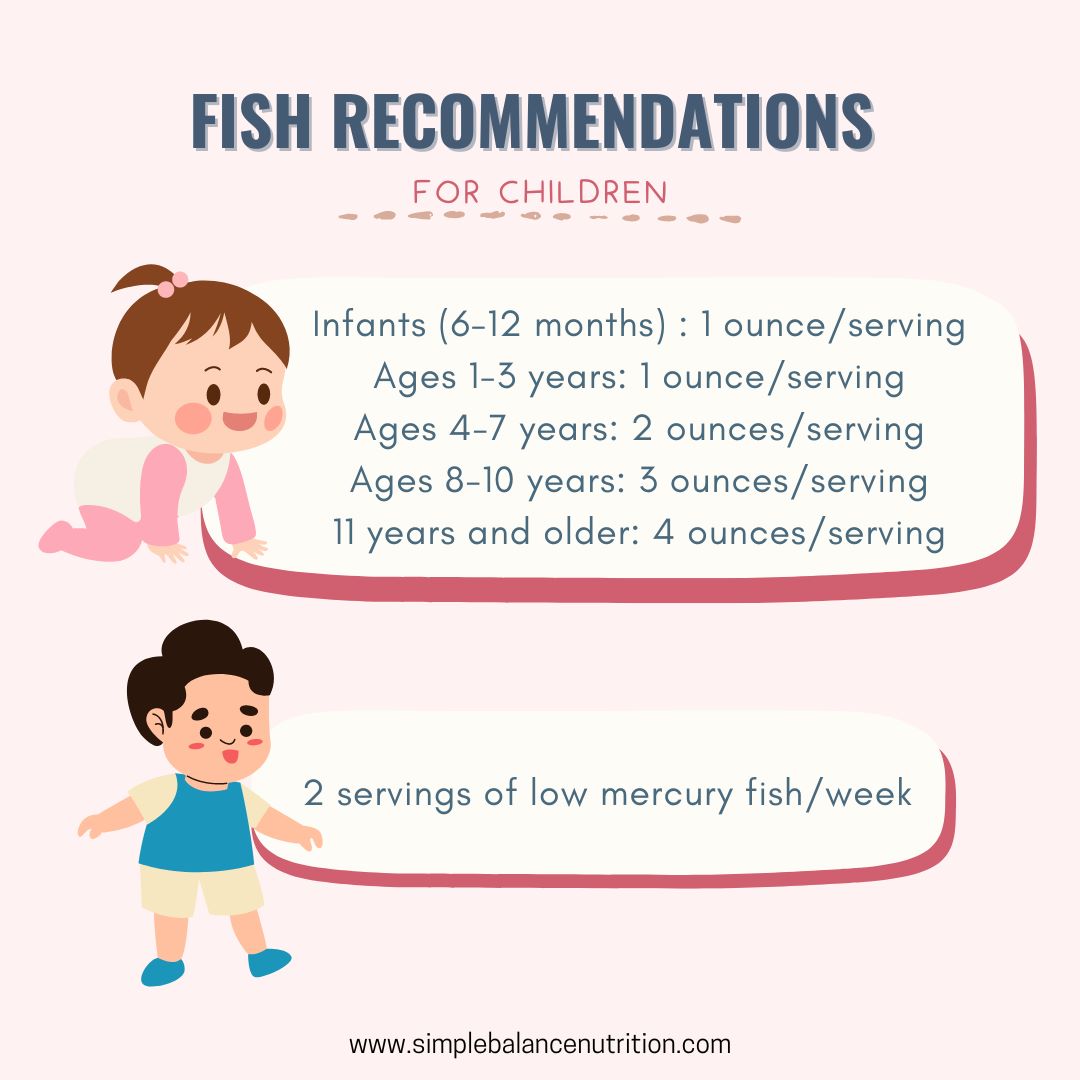
- Offer ultra-low mercury fish weekly, aiming for at least 2 x 1 oz. servings of DHA rich options per week.
- Offer low mercury fish once every two weeks.
- Offer moderately high mercury fish once every month.
- Avoid high mercury fish for babies altogether.
THE FOOD SOURCE OF DHA
DHA is primarily found in fatty fish and shellfish such as salmon, herring, sardines, and trout. However, it’s important to be mindful of mercury levels, especially for pregnant women and children.
High-mercury fish like fresh/frozen tuna (big eye), tilefish, shark, swordfish, king mackerel, marlin, and orange roughy should be completely AVOIDED during pregnancy and up to 2 years old for your baby’s safety.
But don’t worry, there are plenty of low-mercury fish options packed with DHA to help you meet your nutritional needs.
ULTRA LOW-MERCURY FISH
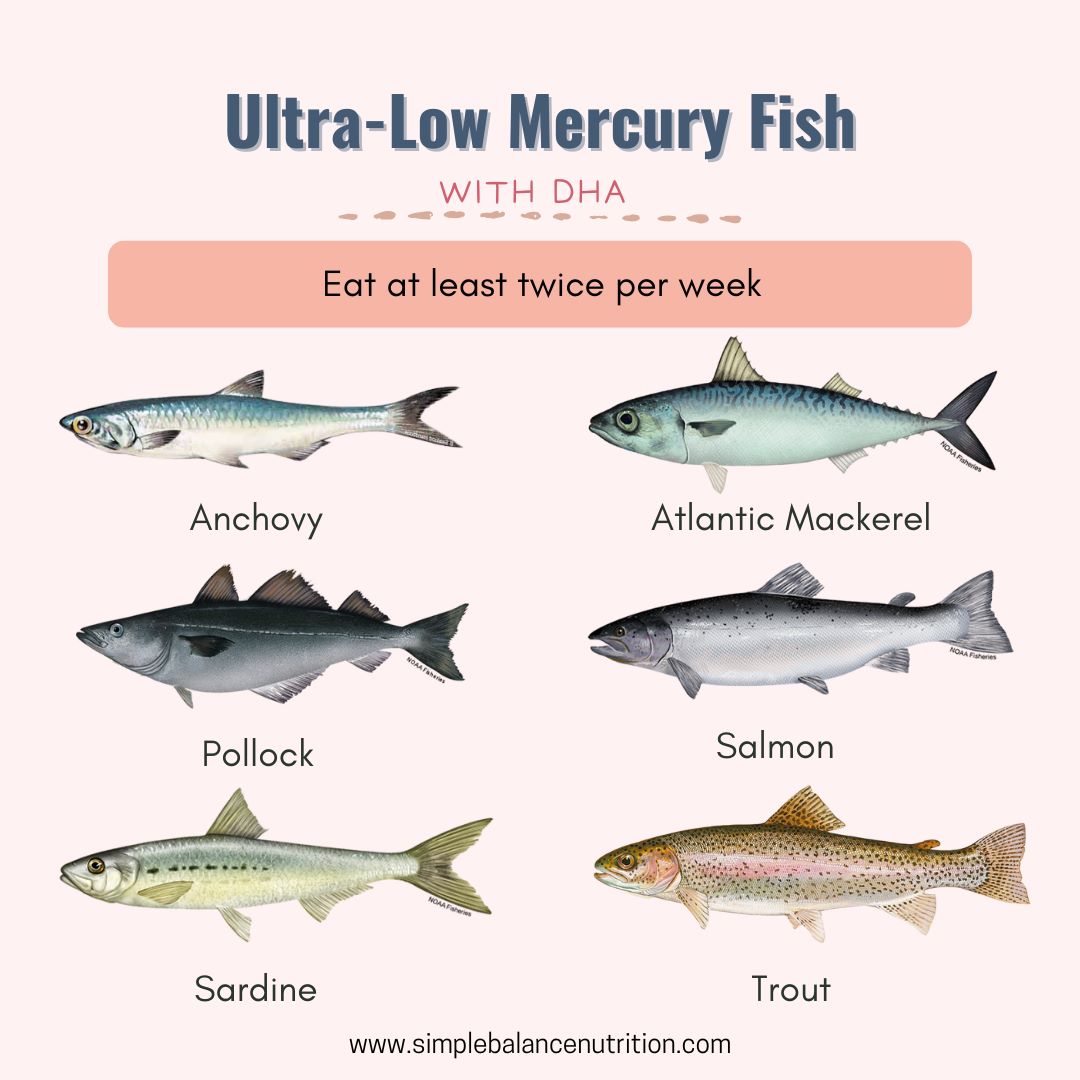
Here are some ultra-low mercury fish (0.06 ppm of mercury or less) and rich in DHA. Offer these fish as often as you like, aiming for at least twice per week.
**The fish in bold are high in DHA with at least 0.4g DHA/100g** (reference)
- Anchovies 江鱼仔
- Atlantic mackerel 大西洋鲭鱼
- Black sea bass 黑鲈鱼
- Butterfish 奶油鱼
- Catfish 鲶鱼
- Clam 蛤蜊
- Crawfish 小龙虾
- Flounder 比目鱼
- Haddock (Atlantic) 黑线鳕
- Mullet 鲻鱼
- Oyster 牡蛎/生蚝
- Plaice 欧蝶鱼
- Pollock 狭鳕
- Salmon (Atlantic farmed, fresh, canned) 三文鱼
- Sardine 沙丁鱼
- Scallop 扇贝
- Shad 西鲱
- Shrimp 虾
- Smelt 胡瓜鱼
- Sole 鳎鱼
- Squid 鱿鱼
- Tilapia 罗非鱼
- Trout, freshwater 淡水鳟鱼
- Whiting 怀廷鱼
LOW MERCURY FISH
Offer low mercury fish (0.07 and 0.15 ppm of mercury) once every two weeks.
- Atlantic croaker
- Cod 鳕鱼
- Crab 螃蟹
- Hake 无须鳕
- Herring 鲱鱼
- Lobster (American and spiny) 龙虾(美洲和刺龙虾)
- Pacific chub mackerel 太平洋黑鲭鱼
- Perch (freshwater and ocean) 鲈鱼(淡水和海洋)
- Pickerel 狗鱼
- Skate 鳐鱼
- Canned light tuna 罐装淡金枪鱼
- Whitefish 白鱼
- Buffalo fish 牛鱼
- Carp 鲤鱼
- Sheepshead 羊头鱼
- Tilefish (Atlantic Ocean) 方头鱼(大西洋)
MODERATELY HIGH MERCURY FISH
Offer moderately high mercury fish (0.16-0.25 ppm) once every month.
- Halibut 大比目鱼
- Mahi mahi 鲯鳅鱼
- Monkfish 安康鱼
- Snapper 红鲷鱼
- Spanish mackerel 西班牙鲭鱼
- Striped bass 条纹鲈鱼
- Weakfish / sea trout 海鲂鱼
HIGH MERCURY FISH
The following fish, with mercury levels between 0.25 and 0.45 ppm, are considered very high in mercury and should be completely avoided for babies and pregnant moms.
- King mackerel 鲭王鱼
- Marlin 枪鱼
- Orange roughy 橙鲷
- Shark 鲨鱼
- Swordfish 剑鱼
- Tilefish (from Gulf of Mexico) 方头鱼(墨西哥湾)
- Big eye tuna 大眼金枪鱼
- Bluefish (Atlantic) 蓝鱼(大西洋)
- Chilean sea bass 智利海鲈鱼
- Grouper 石斑鱼
- Sablefish 黑鳕鱼
- Tuna albacore / white tuna, canned 长鳍金枪鱼 / 白金枪鱼,罐装
- Tuna albacore / white tuna, fresh/frozen 长鳍金枪鱼 / 白金枪鱼,新鲜/冷冻
- Tuna yellowfin 黄鳍金枪鱼
- White croaker / Pacific croaker 白石首鱼 / 太平洋石首鱼
NOT A FISH EATER OR PICKY EATER
If you find it challenging to consume fish regularly during pregnancy or you have a picky eater at home, consider omega-3 enriched eggs, which typically provide 75-100mg of DHA per serving.
FOR FORMULA-FED BABIES

For babies who haven’t started solids yet, they rely on breastmilk or formula for their DHA needs. If you’re breastfeeding, prioritize consuming DHA-rich foods to benefit both you and your baby. If formula feeding, opt for a formula with approximately 11.5 mg/100 mL of DHA, similar to the average level found in breast milk. This ensures your baby receives adequate DHA for healthy development.
EPA+DHA OR DHA ONLY
IF YOU EAT FISH, DO YOU STILL NEED DHA SUPPLEMENTS?

You might wonder if consuming fish provides enough DHA, do you still need to take DHA supplements as part of your plan for nutrition during pregnancy.
Pregnant and lactating women should consume 2-3 servings of a variety of fish weekly. However, even with this recommendation, you may not reach the desired DHA levels. The DHA content varies across fish species, and commonly consumed fish in Malaysia, like Indian mackerel (kembong), anchovies (ikan billis), yellow-tail and yellow-stripe scads (selar kuning), tuna (tongkol), torpedo scads (cincaru), Indian and short-fin scads (selayang), pomfret (bawal), red snapper (merah), king mackerel (tenggiri), merine catfish (jahan) and stingray (pari) have lower DHA levels compared to fish like salmon, herring, or canned white tuna.
In light of this, DHA supplementation offers a convenient solution to ensure you meet your daily DHA requirements. It simplifies monitoring your DHA intake, guaranteeing adequate levels each day, irrespective of variations in fish consumption.
Cod liver oil contains fish oil but because it also contains vitamin A, it should be AVOIDED in pregnancy.
WHAT ABOUT VEGAN?
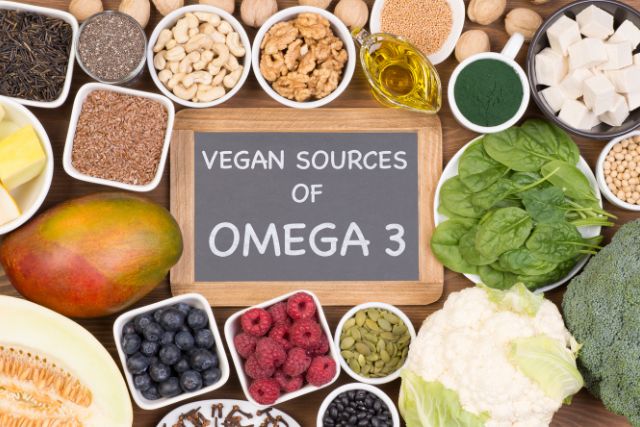
Since fish is not a part of vegan diets and may also be excluded from certain vegetarian diets, obtaining enough DHA solely through diet can be challenging. While fish remains the best source of DHA, there are plant-based alternatives (ALA) such as walnuts and flax seeds that are rich in Omega-3 fatty acids.
Unfortunately, the conversion of ALA to DHA is inefficient, making it difficult to obtain adequate levels solely from plant-based sources. Therefore, I recommend considering an Omega-3 supplement containing at least 200 mg/day to ensure sufficient DHA intake. Additionally, for those following a vegan lifestyle, there are now vegan-friendly DHA supplements (Microalgae Oils) available, derived from algae rather than fish, providing a reliable source of this essential nutrient without compromising dietary preferences.
WHAT ABOUT ALLERGIC TO FISH?

Finned fish and shellfish are considered two different top allergens. Finned fish include species like salmon, cod, and sardines, while shellfish include shrimp, crab, and lobsters.
If your child is allergic to shellfish, it doesn’t necessarily mean they will be allergic to finned fish, as the two are biologically different. Both types of fish should be introduced EARLY and OFTEN when your child shows all signs of developmental readiness for starting solids, typically around six months.
Fish is among the top 9 allergens. For detailed guidance on introducing allergen-containing foods, refer to my post on How to Prevent Food Allergy When Starting Solids.
Also, fish bones can be a choking hazard. Be sure to carefully check for bones when offering fish to your baby!
HOW TO CHOOSE AN OMEGA-3 SUPPLEMENT

There are various omega-3 supplements available on the market, when it comes to choosing an omega-3 supplement for your child, there are several important factors to consider:
1. Quality and Purity
- Third-Party Testing: Ensure the fish oil manufacturer provides documentation of third-party lab results showing the purity levels of their fish oil, down to the particles per trillion level.
- Manufacturing Standards: Check the quality standards the manufacturer uses. Reputable standards include the Norwegian Medicinal Standard, the European Pharmacopoeia Standard, and the Council for Responsible Nutrition’s 2006 monograph. These standards guarantee quality by setting maximum allowances for toxins.
2. Form of the Supplement
- Child-Friendly Forms: Since children often find capsules difficult to swallow, look for omega-3 supplements in the form of jelly, oil, gel capsules, or chewable tablets.
- Gummies Caution: Fish oil gummies are popular, but the typical dosage required to meet daily omega-3 needs might be high, leading to a high sugar intake and potential cavities. Be cautious of this and try to balance with other low-sugar options.
3. Dosage and Safety
- Age Appropriateness: Choose a supplement suitable for your child’s age. Always follow the instructions on the package and do not exceed the suggested dosage.
- Avoid Choking Hazards: For children under 3 years of age, avoid giving capsules as they are a choking hazard. Opt for gummies or liquid forms instead.
4. Source of the Supplement
- Refined Oils vs. Fish Liver Oils: Purchase supplements made from refined oils from the flesh of fish rather than fish livers. Cod liver oils, which contain fish oil, vitamin D, and pre-formed vitamin A (retinol), can be problematic due to the fat-soluble nature of vitamin A. Excessive intake can cause serious health issues. Different brands contain varying amounts of vitamin A, so be mindful of the Recommended Dietary Allowance (RDA) for your child’s age:
-
-
- 1 to 2 years: 250 mcg
- 3 to 6 years: 300 mcg
- 7 to 10 years: 400 mcg
- 10 to 12 years: 575 mcg
-
-
BOTTOM LINE
In addition to their well-known benefits for heart health, cholesterol levels, and brain function, omega-3 fatty acids are especially important during pregnancy and infancy. DHA, a type of omega-3, is vital for the development of the fetal brain and eyes, particularly in the third trimester and early childhood.
Omega-3 fatty acids play a crucial role in promoting various aspects of overall health, including heart health, cholesterol levels, and brain function.
References:
- https://www.canada.ca/en/health-canada/services/food-nutrition/food-safety/chemical-contaminants/environmental-contaminants/mercury/mercury-fish-questions-answers.html
- https://www.who.int/news-room/fact-sheets/detail/mercury-and-health
- https://seafood.oregonstate.edu/sites/agscid7/files/snic/omega-3-content-in-fish.pdf
- https://www.fda.gov/food/consumers/advice-about-eating-fish
- https://www.fda.gov/food/environmental-contaminants-food/mercury-levels-commercial-fish-and-shellfish-1990-2012
Update: August 20, 2025